
In part I, I discussed the mindset about “scale and clean” appointments. In this part, I’ll discuss some clinical tips that have worked for me.
I) Rename the “scale and clean” to “hygiene” appointment.
I am not a psychologist, motivational speaker, or neurolinguistic programming (NLP) practitioner, but I agree that sometimes words can create emotions for us. As mentioned in part I, the phrase “scale and clean” has been overused by dentists and patients, which has been downgraded in the importance of it. From my observations and discussions with other dentists, I think the reason is that the word “clean” subconsciously has a negative or unimportant notation for many people. After all, our parents had nagged us to “clean” up our toys, “clean” the table after eating, and “clean” our rooms when we were young! We didn’t understand the importance of cleaning up and often associated them with unhappy events (e.g. getting yelled at). So, when we emphasise cleaning our teeth regularly, we subconsciously avoid it and downplay the procedure as “just scale and clean”.
Over the years, I have heard many practice-building gurus trying to rename the “scale and clean” appointment to something more positive. A popular term is “Active Matainence” by Dr. Michael Sernik from Prime Speak. I didn’t like it because “matainence” sounded too mechanical and painfully costly to me, such as car matainence. I have re-introduced the name “hygiene” by Ms Sue Rusalen from 7 Figures Hygiene, which I have used for a while. I like it because it sounds more medical and is clear enough for patients to understand what is involved. At the time of this writing, the world was just over the COVID-19 pandemic. Most people understand the importance of personal and hand hygiene. So, the word “hygiene” has somewhat of a positive notation for “helping us to get better.” Furthermore, “hygiene” doesn’t limit the appointment to a procedure but refers to it as a regimen. It allows us (dentists) to discuss other factors that can improve our patient’s oral health, such as deep pocket cleaning, home care, diet, and other modifying factors. I found bringing up other related topics with the patients more challenging if they expected it was “just a scale and clean” appointment.

II) Holding your mirror and scaler differently
Another reason the patients avoid the hygiene appointment is because they fear pain when we remove the calculus. I agree that we can’t perform the procedure utterly pain-free unless we use local anaesthetic. But I believe we can make it less painful or “heavy-handed” by holding our instruments differently and using the appropriate equipment (next point).
In dental school, we had no dental assistants to help us with most of the procedures. We tended to hold our instruments in the middle or close to the working end of the handle because it was natural. But this is also why patients find it painful and heavy-handed when we do our hygiene appointments; the force that we use, for example, to retract the cheek, will fully transfer onto the patients.
Any dentists who practice 4-handed dentistry would agree that holding the mirror at the far end of the handle is much better for at least 2 reasons. Firstly, it is because you don’t have to use a lot of force and can still retract the cheek or tongue sufficiently. Less force means less feeling of push and pull for the patients and less likelihood for us of developing fatigue or carpal tunnel symptoms. Secondly, the dental assistant can adequately see the working field and place the suction correctly. Less water building up in the mouth means a better working view for us and less stress and anxiety for the patient about choking or drowning. More relaxed patients also mean less likely to complain of pain.
Similarly, I also tended to hold the scaler at the far end. The natural tendency is to have it closer to the working end, like a pen, which gives us control of the scaler tip and press/dig it into the calculus. From experience, I found this way is often causing a lot of pain in patients. With the ultrasonic scaler, the scaler tip’s vibration should be able to break the calculus off without pressing hard against it. If I guide the tip at the junction of the calculus and tooth, the bulk of the calculus should break away without too much force. It doesn’t happen if the scaler tip is pointing away or at the bulk part of the calculus. So, I hold my scaler like a probe and apply very light pressure on the calculus. If someone tried to pull the scaler off my hand, there would be no resistance from my hand. Here’s another hint about positioning the scaler tip: I often find newbie dentists digging downwards towards the gingival tissue at the proximal area to remove the calculus buildup. However, it usually required the scaler tip to point upwards at the proximal area to break the calculus due to our hand position.
III) Know your tools
I assume only a few sonic scalers are in use at the time of this writing. Most dental clinics are using ultrasonic scalers. The majority are magnetostrictive, and there is an increase in piezoelectric scalers. Piezoelectric scalers have a slightly higher vibration frequency and more accurate linear pattern, which I found required less power (both machine setting and my hand pressure), less traumatic to the tissue and more comfortable for patients. The main difference is the piezoelectric scalers are effective on the lateral side of the tip. Regardless of which type of scaler we use, remember that tip thickness determines how much calculus we can remove. We can get more subgingivally and proximally the shaper (newer) and narrower the tip. However, there are always parts of the proximal areas that we can’t clean with the scaler tip. A sharp hand sickle scaler and floss are the only way. I like to use the American Eagle Blackjack Pro and M23 because they remain sharp and require no sharpening. Many newbie dentists don’t floss patients’ teeth because they think the combined machine and hand scaling are sufficient. From my observations, apart from the fact that there were always missing spots due to how we angle our hands, the patients also felt better/cleaner if we flossed their teeth, apart from the fact that there were always missing spots. Furthermore, how can we stress the importance of flossing (or interproximal cleaning) if we don’t even floss (demonstrate what we preach) the patient’s teeth ourselves?

IV) Patternisd your clean
As mentioned, many patients fear pain when we perform hygiene appointments. They will be more anxious if we randomly scale back and forth from one area to another. Now, we know that the most common calculus-deposited areas are the lingual surfaces of mandibular teeth. It is also our human nature to be more attentive and less tired at the beginning of the appointment. So, I always start on the lower teeth first because they are the areas that need most of my attention. If I were scaling the lower teeth at the end, my attention would not be as good, and patients would be tired and unable to keep their mouths open, making everyone’s jobs more difficult.
VI) Use the Visual Aid
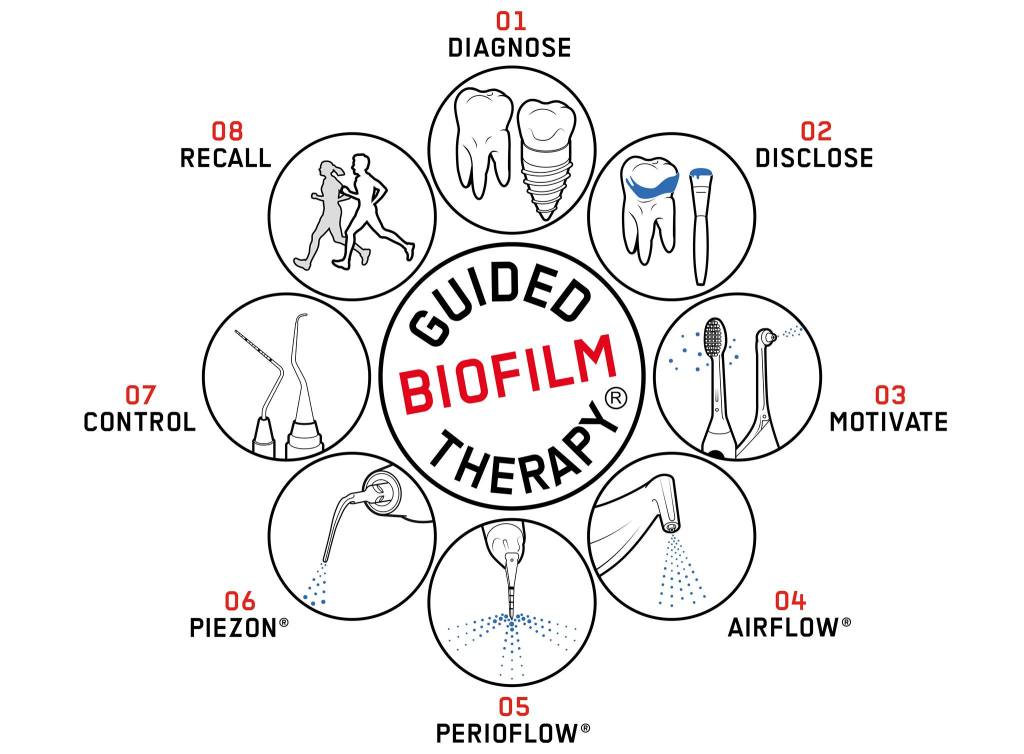
I would be the first to admit that I don’t usually use visual aids. By that, I meant using disclosing solutions. A few years ago, I met a very talented ex-dental hygienist, Ms Sue Rusalen. She re-introduced me to using disclosing solutions based on the principle of Guided Biofilm Therapy (GBT) promoted by EMS Dental. With GBT, disclosing the biofilm not only for patient education but also helps clinicians to clearly see the problem areas instead of blindly going over the whole mouth. With the aid of the Airflow and piezoelectric scaler, it is more efficient and less painful to remove the biofilm and calculus from the teeth.
Another visual aid Sue introduced to me is the light microscope. It is a very old, unappreciated, and ignored concept, but in my opinion, we should all have learned about it in dental school. It is about using the light microscope to screen the harmful pathogens in patients’ biofilm and act on them before diseases occur. It is what medicine and dentistry should be, a proactive/preventive approach rather than reactive/restorative approaches such as fillings and implants. As you should know, as well as the old Chinese proverb saying, “Diseases enter through the mouth”, our job as dentists is not only to improve oral health but also to be the gatekeeper for many systemic diseases. Thanks to all the groundwork done by Ms Sue Rusalen and Dr Tom Larkin, many clinicians (dentists and hygienists) and I could apply The Larkin Protocol easily every day. We now have a subjective tool that can help us accurately assess the patient’s oral health status and the treatment responses, yet simply enough for patients to understand and motivate themselves to participate in the treatment process. I strongly recommend that newbie dentists look up the Larkin Protocol; it would make you become an actual dentist (healer) rather than a specialist repairman.


So, there you go, newbie dentists. These are my clinical tips that have helped me build up my appointment books. Feel free to test them out. I hope they can help you in your practice.
Leave a comment